The ALPS Clinic at NIH has studied autoimmune lymphoproliferative disorders for over 30 years elucidating the genetic underpinnings and natural history of Autoimmune Lymphoproliferative Syndrome (ALPS) due to FAS gene defects (Blood 2014). Over the years, we continue to receive and work-up numerous referrals for diseases that masquerade like ALPS-FAS, presenting with multi-lineage cytopenias due to autoimmune peripheral destruction and splenic sequestration in the setting of non-malignant lymphoproliferation.
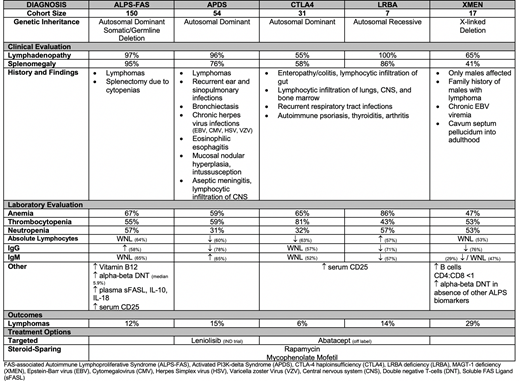
In a review of 259 cases evaluated by our team, there were 150 ALPS-FAS, 54 Activated PI3K-delta Syndrome (APDS), 31 CTLA-4 Haploinsufficiency (CTLA4), 7 LRBA deficiency (LRBA), and 17 MAGT-1 deficiency (XMEN) patients. Non-malignant lymphadenopathy and splenomegaly occurred on average in 83% and 71% of all patients, respectively. Anemia, thrombocytopenia, and neutropenia were seen in 65%, 58%, and 46%, respectively. Thus, autoimmune cytopenias in the setting of non-malignant lymphoproliferation in themselves are not adequate to rule in or rule out a presumptive diagnosis of ALPS-FAS. Timely and accurate genetic diagnosis of ALPS-like conditions will improve the morbidity and mortality associated with these disease processes. Rapamycin, an m-TOR inhibitor provides salutary benefits for many of these conditions by restoring the TREG function and reversing immune-dysregulation. For example, in addition to lymphadenopathy and splenomegaly associated with an increased risk of malignant lymphoma like ALPS-FAS patients, APDS patients usually present with recurrent sinopulmonary and ear infections. Their serum IgM tends to be elevated with low IgG levels. Unlike for ALPS-FAS patients, a potential targeted treatment for APDS exists: Leniolisib, a targeted PI3Kinase p-110 delta inhibitor is currently undergoing clinical trials (Blood 2016).
CTLA-4 is critical for T-cell activation and immune check-point regulation by tempering regulatory T cell function. Patients affected by CTLA4 and LRBA variants present with symptoms of lymphocytic infiltration of the bone marrow (often leading to hypoplastic anemia), gut (colitis, bowel obstruction), lungs (bronchiectasis, restrictive airway disease), and central nervous system (seizures and neurological deficits due to brain and spinal cord lesions). They also tend to have B cell lymphopenia, low IgG and IgM levels. CTLA4 and LRBA patients share pathophysiology as well as clinical phenotype because LRBA gene regulates intracellular lysosomal trafficking and recycling of CTLA-4 protein. Hence CTLA-4 haploinsufficiency or LRBA deficiency renders both patient types CTLA-4 deficient. This can be directly addressed with abatacept infusions, a CTLA-4 hybridized immunoglobulin given as a combination immunosuppressive therapy with rapamycin. Abatacept replaces the CTLA-4 molecule and reverses some of the immune dysregulation and thus morbidity associated with both CTLA4 and LRBA deficiency.
Like APDS patients, XMEN patients are also prone to recurrent ear and sinopulmonary infection, but key differentiating features of this X-linked disorder are that only males are affected, these patients are unable to clear Epstein-Barr virus (EBV) once exposed, and they have a propensity to develop EBV-driven lymphomas. These patients also usually have a strong family history of multiple lymphomas in males. Even though a targeted treatment does not yet exist, steroid-sparing measures such as rituximab, rapamycin and mycophenolate mofetil are the first-line treatments often used in managing their refractory autoimmune cytopenias.
Hence accurate early genetic diagnosis is key to accessing the appropriate treatment, thus decreasing the morbidity and mortality associated with these childhood onset ALPS-like rare inherited disorders (table).
No relevant conflicts of interest to declare.
Rapamycin, Abatacept, Mycophenolate Mofetil.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal